ZeroPSA.com
Doug Kelly MD
Cancer Treatment Centers of America in Phoenix
Douglas.Kelly@ctca-hope.com / ZeroPSA@gmail.com
623.932.8980 Consultation Scheduling
HOME | Post-Op Radiation | Questions & Answers | Diet | Recurrence |Surgery vs Radiation
PROSTATE CANCER RADIATION THERAPY INFORMATION FOR PATIENTS
Contents
Risk Level
Treatment Choices
Surgery vs Radiation
Treatment vs No Treatment
IMRT
SBRT
Brachytherapy
Radiation after Surgery
Radiation for Metastatic Cancer
Hormone Therapy
Marker Seeds and SpaceOAR
Side Effects
Monitoring
Cancer Recurrences
Introduction
Prostate cancer is unique in that there are so different ways to treat it, including not treating. It tends to be a slow-motion cancer, but it can still grow and spread and even kill if enough time passes. Treatments cause a risk of urinary leakage or erectile dysfunction, and who wants to risk those side effects if treatment may not even be not necessary? Deciding between treatments can be gut wrenching. Even trying to decide between different forms of radiation therapy can be difficult. Hopefully this information will help you in your journey to choose a treatment that you are very comfortable with and help you understand the process better!
Risk Level
The first step in choosing a treatment is knowing what risk level your cancer is. This helps guide all treatment choices! The risk level is based mostly on the PSA and Gleason score. The risk level also correlates with stage. Typically low risk = stage 1, intermediate risk = stage 2, high risk = stage 3, and cancer spread to the lymph nodes or bones = stage 4.
| LOW RISK PSA less than 10 and Gleason. 3 + 3 (Grade Group 1) FAVORABLE INTERMEDIATE RISK Gl. 3 + 4 (GG 2) and Less than 50% biopsy cores contain cancer and PSA less than 10 | Treatment Options: Active Surveillance Surgery (radical prostatectomy) Radiation therapy (IMRT or SBRT or Brachytherapy). Only the prostate gland is radiated. |
| UNFAVORABLE INTERMEDIATE RISK Gl. 4 + 3 (GG 3) or Gl. 3 + 4 and 50% or more of biopsy cores contain cancer or Gl. 3 + 4 and PSA is 10 – 20 HIGH RISK Gl. 4 + 4 or higher (GG 4 or 5) or PSA over 20 or Cancer is found breaking out of prostate gland (stage T3 or T4) | Treatment Options: Surgery (radical prostatectomy). May require radiation therapy after. Radiation (IMRT) + hormone therapy. Radiation (IMRT) + brachytherapy boost + hormone therapy. Radiation (IMRT) + SBRT boost + hormone therapy |
There is also a “very low risk” group which is when a case is low risk but only 1 or 2 cores are positive, each core has less than 50% involvement, and the PSA density (PSA divided by gland volume in cc) is less than 0.15. There is also “very high risk” which is for Gl. 5+4 or 5+5, or when six or more cores contain Gl.4+4 or higher, or when there is seminal vesicle invasion. Despite all these risk groups, treatment options can generally be lumped into two categories: favorable or unfavorable.
Lots of Treatment Choices!
For what other cancer can you choose between 13 different treatment options including doing nothing? No other! Treatment choices can be divided into Surveillance, Surgery, Radiation, Ablative, and Hormone Therapy. I won’t talk about surgery much, as the urologist will do that. I won’t talk about the ablative methods as they are uncommon and they can have a tendency to miss some of the cancer if only a portion of the prostate gland is treated. Ablative treatments can be useful if the cancer comes back in the prostate gland after radiation therapy.
Surveillance
| Watchful Waiting | Do nothing. Don’t treat unless the cancer causes symptoms. Consider stopping PSAs and scans. Mostly for men who are elderly and/or have other serious health issues and they probably should not have had a PSA drawn or a prostate biopsy done in the first place. |
| Active Surveillance | Don’t treat initially. Monitor the cancer with regular PSAs, and occasional MRI scans and repeat biopsies. If the cancer seems to grow and reach an important threshold then go on treatment. |
Surgery
| Open Radical Prostatectomy | Traditional surgery, with an open incision in the low abdomen. Can be “nerve sparing”. |
| Laparoscopic / Robotic Prostatectomy | Uses the DaVinci robot or similar, with multiple small puncture sites. Offers shorter recovery times, less blood loss. |
Radiation
| IMRT Intensity Modulated Radiation Therapy | This is standard radiation therapy, also known as “IMRT / IGRT”. It used to take 45 treatments, but now the standard has dropped to approximately 28 treatments. |
| SBRT Stereotactic Body Radiation Therapy | Stereotactic radiation is more precise than IMRT, treating less tissue surrounding the prostate gland, and with only 5 powerful treatments. |
| Proton Therapy | This is an uncommon, very large, and very expensive type of radiation machine which uses protons instead of photons. Studies show no difference in results comparing Protons to IMRT for prostate cancer. It has been shown to be beneficial in pediatric cancers, eye tumors, and base of skull tumors. |
| Brachytherapy Radiation implant | Brachytherapy is a radiation implant, where the radioactivity is placed inside the prostate gland, treating the prostate from the inside-out. Sometimes radioactive seeds are left in the prostate (permanent seed implant), versus sometimes the radiation is given via needles that are temporarily placed into the prostate (HDR brachytherapy) |
Ablative
| Cryotherapy | Needles are placed into the prostate which are cooled and freeze all or part of the prostate gland. |
| High Intensity Focused Ultrasound (HIFU) | A rectal ultrasound creates a highly focused beam that heats up some targeted prostate tissue. |
Hormone Therapy
| Hormone Therapy (HT) | HT given on its own will not cure the cancer, but can put the cancer into remission. However, combined with radiation it can increase the cure rate for high risk cancers. Also known as Lupron or Eligard. |
Surgery versus Radiation – Which one to Choose??
Surgery vs Radiation is often the ultimate question men with prostate cancer face. Obviously you hope to pick the treatment that will cure your cancer but which will also result in the least pain, suffering, expense, and side effects. Please see my page Surgery vs Radiation for my take on this.
Treatment versus No Treatment (Active Surveillance)
Which prostate cancer treatment does not cause physical side effects? Active Surveillance! How many men die from their prostate cancer within 5 years of diagnosis? Only 1% ! It is truly a slow-motion cancer in many cases. Put these facts together and many men are intrigued by the idea of putting off treatment and monitoring the cancer for a while to see if it shows aggressive behavior which would warrant going on treatment.
Usually a urologist will follow patients on active surveillance. A PSA is repeated every 3 – 6 months. A rectal exam (DRE) is done every year. A biopsy is recommended 6 – 12 months after the first biopsy, and then every 2 – 5 years after that, or sooner if the PSA jumps. Repeat MRI scans may also occasionally be done, especially before repeat biopsies.
Active surveillance is probably best for men with stage 1 low risk prostate cancer, i.e. those who have Gleason 3 + 3 and a PSA less than 10. Ideally there will be less than 50% of biopsy cores that show cancer, and ideally no core will have greater than 50% cancer involvement. Patient age is ideally 60s or 70s. These are not strict rules.
Active surveillance is not for everyone. You must be psychologically at peace with having an untreated cancer in your body, even if it is slow growing. You need to get repeat prostate biopsies occasionally, which are painful and have risks. The PSA may naturally bounce up and down which will scare you on occasions when it rises. The cancer will tend to grow with time. It may grow to a point where the treatment required is more aggressive or the cure rate is lower. Overall about half of all men on active surveillance will end up having treatment within 5 years of starting the program.
Active surveillance would not exist if we had a magic bullet treatment, ie a treatment with a high chance of cure and a low risk of side effects. You know what reminds me of a magic bullet? Radiation therapy.
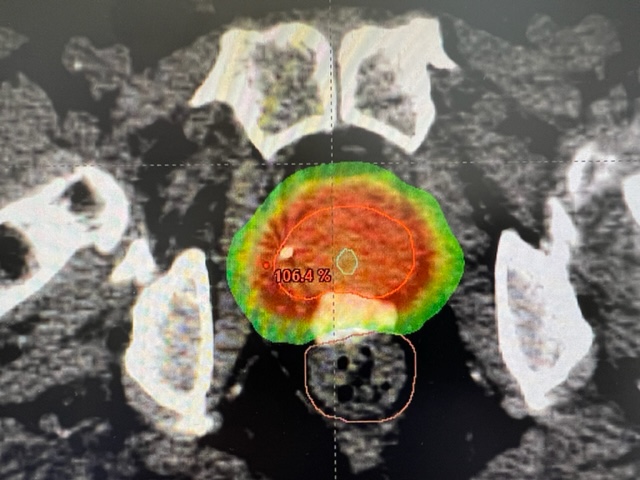
Intensity Modulated Radiation Therapy (IMRT / IGRT)
This is the most common form of prostate radiation in the US. Depending on risk level we can choose to treat just the prostate gland for low – favorable intermediate risk, the prostate + seminal vesicles for unfavorable intermediate risk, or the prostate + seminal vesicles + pelvic lymph nodes for high risk. For aggressive cases we also combine hormone therapy with radiation in order to increase the cure rate. Traditionally IMRT was given at a low dose for 45 treatments, given 5 days a week for 9 weeks. Recent studies have found that 28 treatments given at a higher dose per day gives the same cure rate and side effects as 45 treatments, so 28 has become the new national norm. With IMRT the radiation beams enter the body from many different angles, preferentially from angles that avoid healthy organs like the bladder and rectum, each beam is shaped to match the shape of the target from that particular angle, and each beam is broken up into little “beamlets” of varying intensity.
Stereotactic Body Radiation Therapy (SBRT)
Stereotactic radiation is one of the newest and most promising forms of radiation, and it is a favorite of mine. Whereas radiation used to take 45 treatments this only requires 5 treatments! Perhaps you have come across the term “CyberKnife”. That was one of the original machines used for SBRT, but now SBRT can be done equally well by many other machines such as TrueBeam, Trilogy, and Tomotherapy to name a few. SBRT uses IMRT technology, but it differs from IMRT in that less tissue surrounding the prostate gland is included in the treatment field. We usually do not include the lymph nodes. A much higher radiation dose per treatment is used. The physician is called to the treatment console for every treatment to supervise that the treatment is lined up perfectly. Treatments take about 30 minutes and are usually given every second day.
So why don’t we recommend SBRT for everyone? For many reasons. SBRT is only approved for low risk or favorable intermediate risk prostate cancers, and it may be under-treatment for more advanced cancers. SBRT is a newer treatment than IMRT, so there are less long-term results available. There are only a few 10-year results out which are excellent. Some patients or doctors may prefer the more proven IMRT. SBRT has been found to cause more short term urinary side effects than for IMRT – the side effects tend to come on earlier and the severity may spike higher. For this reason, we typically don’t recommend SBRT for patients with very large prostate glands, a lot of urinary symptoms, or those who have had a prior TURP. Finally, marker seeds and hydrogel are more critical to use and a patient should be able to safely undergo that procedure. The HYPO-RT-PC study compared SBRT to IMRT and found they both had the same cure rate. Early side effects were “more pronounced” with SBRT but in the long term they were equal.
SBRT is certainly one of the fastest and easiest ways to treat prostate cancer. For out-of-state patients we can accomplish the entire preparation and treatment in 15 days. Our “Fast Track schedule” looks like this:
Day 1 Friday: Place gold marker seeds and SpaceOAR hydrogel.
Day 4 Monday: Mapping with CT-simulation and often an MRI of the pelvis.
Days 7,8,11,13,15 Thu, Fri, Mon, Wed, Fri: Treatments. Can go home right after the final treatment!
SBRT Boost
A “Boost” means giving additional radiation to a smaller area, usually focused on the area of greatest concern. Although SBRT by itself is not recommended for unfavorable prostate cancer, we can use an SBRT boost to deliver part of the radiation with SBRT, and part with IMRT. Typically I would do 3 treatments with SBRT, and follow this with 25 days of IMRT to the prostate, seminal vesicles, and the pelvic lymph nodes. The grand total is still 28 treatments. I would consider this treatment to be more aggressive than standard IMRT as a higher dose can be given to the prostate. However, there is one treatment which is probably stronger, the Brachytherapy Boost.
Brachytherapy Boost
For high-risk prostate cancer there has been a trend to recommending “triple therapy” with hormone therapy + brachytherapy + 25 days of IMRT to the prostate, seminal vesicles, and pelvic lymph nodes. Studies show this gives the highest success rate for high-risk prostate cancer. In the ASCENDE-RT study 80% of the men in the brachytherapy boost group were still cancer-free 15 years after treatment, whereas only 53% of the men receiving standard IMRT without brachytherapy were cancer free. An HDR brachytherapy boost involves general anesthetic. Up to twenty needles are inserted through the perineum (the skin between the anus and testicles). A CT scan is taken and a computer plan generated. The needles are hooked up to a brachytherapy machine which pushes a highly radioactive pellet into each needle one-by-one, controlling where in each needle the pellet will rest for a while, and how many seconds it will rest for. The needles are then pulled out. The whole process from the start of placing the needles until the time the needles are removes takes about 4 hours. I use the brachytherapy boost first, then about 1 – 2 weeks later the pelvic IMRT radiation is started.
Radiation after Surgery
I have a separate page which talks about radiation after surgery. Sometimes radiation therapy is recommended after radical prostatectomy. Typical reasons might be that the PSA does not drop all the way to 0.0, or the PSA has begun to rise after surgery, or cancer was found in the lymph nodes at the time of surgery. In these cases we may give radiation therapy to the area of the pelvis where the prostate and seminal vesicles used to be. This is known as the “prostate surgical bed”. Often we include the pelvic lymph nodes as well. We also frequently combine some hormone therapy for 6 – 12 months with the radiation therapy. The SPPORT trial found a benefit to adding lymph node radiation and short term hormone therapy to the prostate bed radiation. When we give radiation after surgery we usually need to go at a slower rate, and typically 38 – 39 treatments are required. SBRT cannot be used. Marker seeds and hydrogel are typically not used.
Radiation for Metastatic Prostate Cancer
When cancer has metastasized to the bones, the main treatment is hormone therapy. However, there are cases where we still use radiation therapy: 1) If the cancer has spread to the bones and is painful then we will often offer 1 – 10 radiation treatments to the painful bone areas. 2) If there is very limited spread to the bones in three spots or less, we will sometimes radiate the prostate gland, as this has been shown in the STAMPEDE trial to help prevent additional metastases from developing and helped patients lived longer. Often 5 treatments of SBRT are used. 3) If there has been previous prostate cancer treatment with radiation or surgery, and the cancer has come back in only a few lymph nodes or bones, this is called “oligometastatic cancer”. There may be a benefit to giving SBRT to the few metastases.
Hormone Therapy
Hormone Therapy is usually added for unfavorable intermediate or high risk cases. This is typically given via injections of Lupron or Eligard. These medications reduce the testosterone in your body, causing the prostate cancer to shrink and the PSA to drop. Hormone therapy given as the sole treatment can put the cancer in remission, but it cannot cure the cancer. However by combining hormone therapy with radiation therapy we can increase the increase the cure rate over what we would achieve by just giving radiation therapy on its own. Casodex (bicalutamide) tablets are often prescribed for 30 days along with the first injection of Lupron / Eligard. The injections come in 1, 3, 4, and 6 month strengths. Hormone therapy is typically prescribed for 4 – 6 months total for unfavorable intermediate prostate cancer, and for 12 – 36 months for high risk prostate cancer. Side effects of these injections are caused by the resultant low testosterone level and the side effects will usually go away once the injections are stopped and the testosterone level rises back into the normal range. Side effects include hot flashes, erectile dysfunction, low sex drive, weight gain, fatigue. With long term use there can be osteoporosis (thinning of bones). Studies show that daily exercise can reduce some of the side effects. In addition eating a low carbohydrate diet (such as Atkins) can reverse the weight gain from hormone therapy. Some studies also suggest patients may respond better and longer to hormone therapy if they are on a low carb diet.
Marker Seeds and SpaceOAR
Marker seeds and SpaceOAR hydrogel are usually inserted into the prostate area before radiation treatment. Three marker seeds are injected into the prostate gland, which will help the therapists precisely line up the radiation treatment every day.
This is a minor surgical procedure in which general anesthetic is used. You will need to take antibiotic tablets for three days starting the evening before the procedure. You will need to stop all NSAIDS, aspirin, and blood thinners 7 days before the procedure. You need to eat nothing after midnight, do an enema in the morning, and have someone drive you home.
To perform the procedure an ultrasound is placed into the rectum and we can see the prostate gland on the ultrasound monitor. We then insert a needle through the perineum, which is the patch of skin in between the anus and the testicles. Markers seeds are injected into the upper prostate (which is called the base) and into the lower prostate (which is called the apex). These marker seeds are smaller than a grain of rice. They will remain in the body permanently. They do not react with the body tissues. The marker seed locations do not necessarily correspond to locations of the cancer, and the daily radiation treatments are not aimed at the marker seeds – the seeds help ensure the entire prostate gland is lined up properly for treatment each day. During the same procedure SpaceOAR hydrogel is also utilized. A needle is placed through the perineum and advanced into the narrow space in between the rectum and prostate. 10cc of hydrogel (about 1/3 of an ounce) is then injected into this space. The gel pushes the rectum and prostate apart and the gel hardens. By increasing the space in between the prostate and rectum fewer radiation beams will pass through the rectum during treatment and there will be less rectal side effects. Studies also show a reduction in erectile dysfunction with the use of hydrogel. The hydrogel starts to break down three months after it has been injected, eventually disappearing. Hydrogel can occasionally cause some rectal discomfort.
Mapping / CT-Simulation / Computer Planning
Before radiation therapy can start we must perform a CT-simulation. We construct a vacuum-cushion that will hold you still during treatment, then a CT scan of the pelvis is done. No contrast is required. A few marks are placed on the skin. For the simulation and for the treatment we will advise the patient to consume 2 cups of water 30 minutes prior in order to have a comfortably full bladder. If possible the rectum should be empty-ish from a bowel movement earlier in the day. A simulation appointment takes about 30 minutes. Sometimes an MRI scan of the pelvis will also be performed on the same day as the simulation. Next we design a treatment plan on the computer. This does not require any participation from you! It takes 2 – 7 days to create and QA test a computer plan, then we are ready to start treatment on you.
Side Effects of Radiation
Radiation treatments cause both short term and long term side effects. The difference causes, time onset, and symptoms are described below. Typically side effects are mild
| Short Term Side Effects Occur due to inflammation. Start a few days to a few weeks after radiation therapy begins. Typically go away within 6 weeks of radiation ending. | Urinary tract irritation causing discomfort, burning, slower stream, more frequent urination. 80% chance. Increased bowel movement frequency, mucous, diarrhea. 30% chance. Minor urine leakage may occasionally occur. The need for a urine catheter may occur in 1%. |
| Long Term Side Effects Occur due to internal scar tissue (fibrosis). May begin 6 months – 5 years after radiation ends. May become chronic or lifelong conditions. | Weakening of the erections which may ultimately become “erectile dysfunction” in 33% of men. Some narrowing or scarring of the urine passage, ie the urethra. May require a procedure to widen the urethra in 5% of cases. Rectal or bladder bleeding (rare, less than 2%) Urinary incontinence (rare, less than 2%) Secondary cancers (rare, less than 1%) |
For short term urinary symptoms we often prescribe Flomax (tamsulosin) to help the urine flow. Azo (pyridium) can reduce burning symptoms. For diarrhea we prescribe Imodium-AD, and sometimes a low fiber (low residue) diet can be helpful. Regarding erectile dysfunction, a prescription for Viagra or Cialis can be helpful.
There is typically no down time during radiation and most patients can continue working during and after the treatment course.
Monitoring
We monitor the cancer with PSA blood tests. We do not routinely do any follow-up scans or biopsies unless the PSA starts to rise significantly. We don’t typically check the PSA during radiation as the treatment can inflame the prostate and may cause the PSA to temporarily rise. The first PSA is taken 3 months after the treatment is completed or when the next Lupron injection is due, and the PSA should be decreasing. We check the PSA every 6 months after that. The PSA will continue to decrease for 5 years or more and may eventually drop down to as low as 0.1 or 0.2. There is no official “normal” range for PSA after radiation, but I often say that a PSA below 1 is normal. Sometimes the PSA can bounce up and down a little after treatment. It is the overall trend we look at.
What Happens if the Cancer Comes Back?
There is a separate page on this website devoted to cancer recurrence. We become alarmed when the PSA climbs on three consecutive measurements. The official definition of radiation failure is if the PSA ever rises to 2 points higher than the lowest measurement obtained since the treatment ended. If that happens we may recommend some repeat scans such a CT scan, bone scan, and/or a PET scan. A rising PSA would be the first sign of a problem. Prostate cancer can come back in the bones, lymph nodes, or the prostate gland, and the PSA will rise in any of those situations. Sometimes we will do another prostate biopsy. After analyzing all the test results we end up with one of the following scenarios:
| Types of Cancer Recurrence | Treatment Options |
| PSA Recurrence Only Scans are all clear! Don’t know where the cancer is coming back. Sometimes it’s a false alarm and the PSA will drop back down on its own. | If there has not been a prostate biopsy then consider doing one. Continue PSA surveillance, and rescan every 3 – 6 months if the PSA rises further. Intermittent hormone therapy (cycle on and off the Lupron) |
| Pure Local (Prostate) Recurrence Recurrence found in the prostate gland only, not found anywhere else | Surveillance (do nothing) Intermittent hormone therapy Cryotherapy (freeze the prostate) HIFU (high intensity focused ultrasound |
| Metastatic Recurrence Recurrence found in the bones or lymph nodes | Continuous hormone therapy A referral to a medical oncologist may be requested. |
| Oligometastatic Recurrence Isolated recurrence found in only a couple bones or a couple lymph nodes (oligo-metastatic recurrence) | Stereotactic radiation (SBRT) to the few metastases. Hormone therapy x 6 – 12 months is typically combined with the SBRT. |
A common thing you may hear from urologists is that “you can’t have surgery if the cancer comes back after you have had radiation”. This is true, but the only situation where that becomes an issue is in the situation of a Pure Local Prostate Recurrence, and there still are other treatment options available! In a 10-year SBRT study by Katz, he found that a prostate recurrence happened in less than 2% of patients.
Conclusion
Good luck in your journey! I’m a radiation oncologist and I happen to believe that radiation therapy is a great option for many men!